A birth control option that prevents pregnancy for up to 10 years while also giving you shorter periods sounds too good to be true. But that's exactly what IUDs deliver.
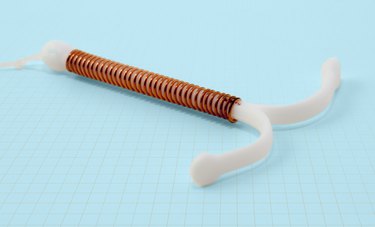
An intrauterine device, commonly referred to as an IUD, is a popular form of birth control inserted into the uterus. It's highly effective and provides long-lasting pregnancy prevention. But that's not the only benefit the device offers. IUDs can also regulate or eliminate menstrual cycles, lessening negative period symptoms like painful cramping and heavy bleeding.
Video of the Day
Video of the Day
The use of IUDs as a birth control method is growing. More than 10 percent of women in the U.S. ages 15 to 49 used an IUD or a birth control implant from 2017 to 2019 compared to just over 5 percent from 2006 to 2008, according to the Centers for Disease Control and Prevention (CDC). [Note: The LIVESTRONG.com team makes deliberate choices about the language we use when it comes to sex and gender. Anyone with a uterus can use an IUD to prevent pregnancy, but the CDC still categorizes people who do as women, so we've used that language here.]
That growth in IUD use is due, at least in part, to the fact that the small T-shaped device now comes in different forms: hormonal and non-hormonal.
"The benefits of the hormonal IUDs have really moved them up in line of preference," says Maria Tucker, MD, an ob-gyn at the Einstein Montgomery Medical Center. "With birth control pills you'll still get a menstrual period, but with the hormonal IUD most women have no period at all. That's a benefit."
IUDs approved by the Food and Drug Administration (FDA) include the hormonal IUDs Kyleena, Liletta, Mirena and Skyla and the non-hormonal copper IUD Paragard. The length of effectiveness depends on the type of IUD a person chooses, but some IUDs can last for up to 10 years.
Comparing IUD Options
Brand Name | Efficacy | When It Starts Working | Size | Hormone Dose |
|---|---|---|---|---|
Skyla | 3 years | 7 days post-insertion | 28 x 30 mm | 13.5 mg |
Kyleena | 5 years | 7 days post-insertion | 28 x 30 mm | 19.5 mg |
Liletta | 6 years | 7 days post-insertion | 32 x 32 mm | 52 mg |
Mirena | 6 years | 7 days post-insertion | 32 x 32 mm | 52 mg |
Paragard | 10 years | Immediately | 32 x 36 mm | Non-hormonal |
Here's how an IUD works: When a hormonal IUD is inserted into the uterus, it releases small amounts of the synthetic hormone progestin — not to be confused with progesterone, the hormone our bodies make naturally.
The progestin prevents ovulation and changes the cervical mucus and uterine lining in ways that prevent pregnancy, according to Planned Parenthood. With this hormonal method, people can also see a difference in period pain and menstrual cycle frequency.
The non-hormonal option, the copper IUD, creates a toxic environment for pregnancy, according to ob-gyn Christine Greves, MD. This means the uterus becomes an unsuitable environment for a pregnancy to occur. It can potentially cause different side effects, like heavier periods.
"The IUD, depending on which one it is, creates a hostile environment so the sperm cannot reach the egg," says Janine Barsoum, MD, ob-gyn. "When that occurs, you won't have fertilization."
Before making the decision to have an IUD inserted, it's a good idea to discuss options with your doctor and talk through any specific questions and concerns you may have. In the meantime, here are a few things ob-gyns want you to know about IUDs.
1. An IUD Is Not Permanent
Given the long-lasting effectiveness of IUDs, it's a common misconception that having one inserted comes with a long-term commitment. That's not the case, according to Dr. Greves, a women's health educator in Central Florida. You're allowed to change your mind if an IUD no longer feels like the right choice.
"It is super easy to remove them," Dr. Greves tells LIVESTRONG.com.
Let's say plans have changed and a person is interested in getting pregnant, or just wants the IUD out of their body. The first step is contacting your doctor and scheduling an appointment for removal.
At your appointment, you'll lie back and place your feet in stirrups, the same position as insertion. Then a doctor or nurse will gently pull on the IUD string and the device should slip out. It's possible you'll feel slight cramping as it's removed.
2. Insertion Can Be Uncomfortable, but It’s Temporary
Many of us have heard IUD insertion horror stories. The pain factor when it comes to getting an IUD is probably the most frequent worry doctors hear from their patients.
And there very well may be some discomfort — but it's usually over quickly. "The biggest thing is setting expectations," Dr. Tucker says. "We let patients know that this can be a little uncomfortable, but it will pass."
Take an over-the-counter pain reliever like ibuprofen or Tylenol to prevent some of the pain at least an hour before insertion, Dr. Greves says.
Your doctor might also give you a numbing medicine on the day of your appointment. "Some doctors may infuse a little bit of lidocaine into the uterus, or do a nerve block like what you'd get at the dentist," Dr. Tucker says.
If you feel comfortable chatting with your ob-gyn, distract yourself from the insertion by carrying on a conversation.
Despite the less than pleasurable experience, for most people, the benefits outweigh the brief discomfort. "It is uncomfortable, but it's a lot less uncomfortable than dealing with the possible consequences if you don't have the IUD, like a painful period or an unwanted pregnancy," Dr. Greves says.
3. Yes, Side Effects Are Possible
Worried about how an IUD will make you feel? Side effects are possible, but it also depends on the type of IUD inserted — and some people don't experience any side effects at all.
According to Dr. Barsoum, common side effects from a hormonal IUD include:
- Light cramping and backaches after initial insertion
- Irregular periods
- Spotty bleeding
"The copper IUD has no hormones, so it doesn't have these issues," Dr. Barsoum says, but it does have its own set of potential side effects, including:
- Heavier or longer periods
- More or worse cramps
- Irregular periods
"The progestin-only IUD also has some people believe it can cause weight gain or hair loss. Less than 5 percent of patients who have an IUD placed actually have any sort of weight gain with the IUD," Dr. Barsoum says.
If weight gain does occur, it's typically in small amounts. "Maybe 5 to 7 pounds, not something like 20 pounds, but it's very person-dependent," Dr. Barsoum says.
4. Safety Risks Are Rare
Having a foreign object placed inside your body is reason for possible concern, but IUDs are not only highly effective but also safe. There are limited risks associated with insertion that only occur rarely.
"When placing the IUD, there are always risks," Dr. Greves says. "It's called uterus perforation. It's when the IUD goes through the wall of the uterus. That can occur, but it happens very, very rarely."
In fact, the complication happens in just 1 per 1,000 insertions, according to a March 2016 review in Open Access Journal of Contraception.
Other complications can include the IUD falling out or being rejected by the uterus, which are also rare.
"Some women are concerned that they can't use a tampon with an IUD," Dr. Tucker says. "The way the string is left in place, it's rare that it would get stuck with a tampon. There's a reason we leave the string very short."
"With education and explanation, we still believe in the safety of IUDs. The benefits of the IUD outweigh the risks," Dr. Tucker says.
Related Reading
5. IUDs Will Not Cause Infertility
Another big reason for hesitancy toward IUDs is the belief that they could affect future family planning. The truth is, an IUD has no effect on a person's ability to get pregnant later on.
"There is no risk of fertility issues related to IUD use," Dr. Barsoum says.
Scientific research dating back to the 1980s backs up those claims. In a December 1986 report from the World Health Organization, researchers found fertility returned immediately once an IUD was removed.
In more recent research, the same conclusions have been made. A July 2018 study in Contraception and Reproductive Medicine found IUDs do not negatively affect a person's fertility after removal, regardless of the type and how long it's used.
If a person does have trouble getting pregnant, it's more likely there are other factors causing the issue. "It's probably not the IUD, but other things that haven't been explored," Dr. Greves says.
Those unexplored underlying issues could include fibroids or endometriosis, Dr. Barsoum says. "We treat issues that can have fertility implications with IUDs, but it's not the IUD itself that causes infertility."
6. IUDs Do Not Cause Abortion
The misconception that IUDs cause abortion is 100 percent untrue.
"It works by making the uterus an unfriendly environment for a pregnancy," Dr. Greves says. "It does not cause an abortion."
Once an IUD is placed correctly, a pregnancy cannot occur, meaning an IUD causing abortion is impossible.
In the rare chance the IUD fails and pregnancy happens, your doctor will likely remove the device. Less than 1 percent of people with hormonal and non-hormonal IUDs become pregnant each year, according to Dr. Barsoum.
"An IUD cannot terminate a pregnancy. It prevents pregnancy," Dr. Barsoum says.
- Centers for Disease Control and Prevention: "Contraceptive Use"
- Office on Women's Health: "Birth control methods"
- World Health Organization: "Mechanism of action, safety and efficacy of intrauterine devices"
- Contraception and Reproductive Medicine: "Return of fertility after discontinuation of contraception"
- Michigan Medicine University of Michigan: "Comparing Intrauterine Devices (IUD)"
- Centers for Disease Control and Prevention: "Use of Contraception in the United States: 1982–2008"
- National Library of Medicine: "Progestin-Only (norethindrone) Oral Contraceptives"
- Planned Parenthood: "What are the side effects of IUDs?"
- Open Access Journal of Contraception: "Intrauterine devices and risk of uterine perforation: current perspectives"
Is this an emergency? If you are experiencing serious medical symptoms, please see the National Library of Medicine’s list of signs you need emergency medical attention or call 911.